VACCINES AND VITAMIN D: MEASURING IMMUNE RESPONSES
by Associate Professor Dr Cheng Siang Tan
Institute of Medicine and Health Sciences
Institute of Medicine and Health Sciences

Researchers in Sarawak, Malaysia, measured the immunity responses of people who received different COVID-19 vaccines.
The rapid international effort to develop and deploy vaccinations against the SARS-CoV-2 virus has been a saving grace of the pandemic. But it's not over yet. Scientists now need to understand in detail how our immune systems respond to the different vaccines over time to continue to tweak them and improve their efficacy as the virus changes.
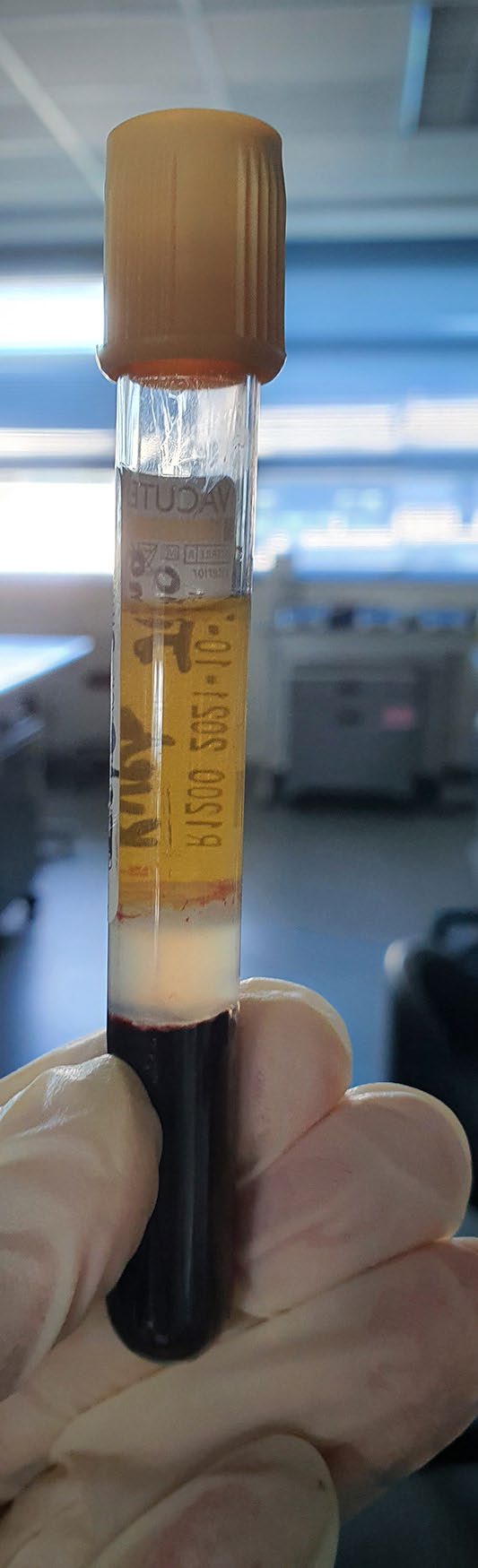
In a paper published in Scientific Reports, researchers at UNIMAS analysed blood samples of more than 300 vaccines in the state of Sarawak. They tested for the appearance of various antibodies up to 13 weeks after receiving the second dose of two different types of vaccines: the Pfizer/BioNTech and Sinovac vaccines. Each vaccine uses a different approach to elicit an immune reaction. The Pfizer/BioNTech vaccine contains mRNA that codes for the spike protein present on the surgace of the SARS-CoV-2 virus. When a person's cells start producing this protein, the immune system responds by forming antibodies that can recognize and bind to it, preventing the virus from attacking host cells. The Sinovac vaccine is made using whole inactivated virus, stimulating broad immune response.
In a nearby lab at the Department of Chemical Engineering and Energy Sustainability, Professor Dr Mohammad Omar Abdullah and his colleagues have made solid catalysts for biodiesel production using waste ginger leaves.
The production and use of biodiesel have increased significantly in recent years. The production process involves converting oils and fats into fatty acid methylester, the predominant compound in biodiesel. Currently, the catalysts used in this chemical reaction are in the same phase as their reactants; in this case the oil and catalysts are both in liquid form. But it is expensive to separate the catalysts afterwards for reuse.
The production and use of biodiesel have increased significantly in recent years. The production process involves converting oils and fats into fatty acid methylester, the predominant compound in biodiesel. Currently, the catalysts used in this chemical reaction are in the same phase as their reactants; in this case the oil and catalysts are both in liquid form. But it is expensive to separate the catalysts afterwards for reuse.
Malaysian national statistics show very low rates of intensive care admission (0.0066%) and death (0.01%) among people who received both doses of any vaccine. However, the statistics also show that, relative to Pfizer/BioNTech recipients, Sinovac vaccines were more likely to require intensive care (5.5 times) or die (3 times).
Interestingly, the UNIMAS study found that a small percentage of people (1.9%) who received the Sinovac vaccine failed to produce antibodies against the virus's spike protein three weeks after the second dose, while 2.9% had very low antibody levels at week 13. "This could explain why COVID-19-related deaths are relatively higher among Sinovac recipients," says Tan.
The team also wanted to test whether vitamin D insufficiency has an effect on a person's ability to develop a strong immune response following vaccination against SARS-CoV-2.
They were surprised to find that only 13.4% of the study population had sufficient vitamin D levels, despite Malaysia's location near the equator. This could be because people stayed indoors during lockdowns.
Interestingly, the UNIMAS study found that a small percentage of people (1.9%) who received the Sinovac vaccine failed to produce antibodies against the virus's spike protein three weeks after the second dose, while 2.9% had very low antibody levels at week 13. "This could explain why COVID-19-related deaths are relatively higher among Sinovac recipients," says Tan.
The team also wanted to test whether vitamin D insufficiency has an effect on a person's ability to develop a strong immune response following vaccination against SARS-CoV-2.
They were surprised to find that only 13.4% of the study population had sufficient vitamin D levels, despite Malaysia's location near the equator. This could be because people stayed indoors during lockdowns.
"Interestingly, we found that the magnitude and longevity of antibodies were not dependent on serum vitamin D levels," says Tan.
The team says its findings support a three-month interval between the second dose and the following booster of the Sinovac vaccine, but that recipients of the Pfizer/BioNTech vaccine, who have significantly higher antibody levels could wait longer.
Next, the team plans to compare antibody responses in people receiving booster doses of the same or a different vaccine.
The team says its findings support a three-month interval between the second dose and the following booster of the Sinovac vaccine, but that recipients of the Pfizer/BioNTech vaccine, who have significantly higher antibody levels could wait longer.
Next, the team plans to compare antibody responses in people receiving booster doses of the same or a different vaccine.



